Our patented technology creates an accurate and transparent picture of patient data, leading to improved quality reporting.
TECHNOLOGY
Healthcare CDI Software Coded for Financial Success
How It Works
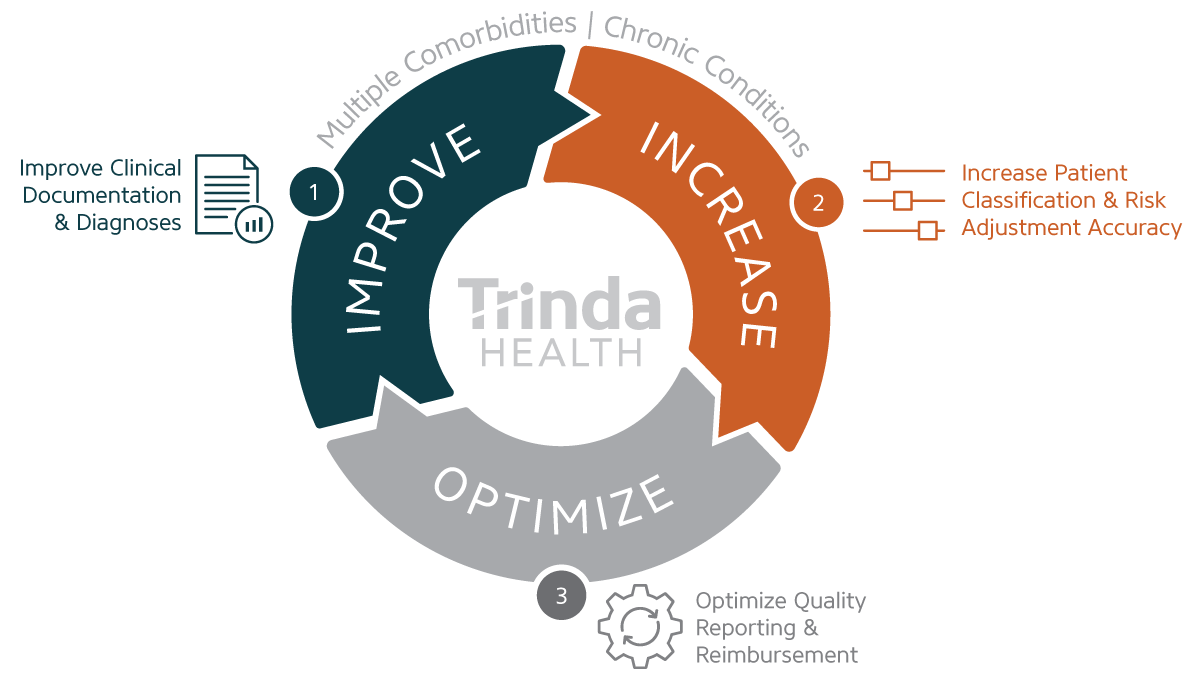
1. Improve Clinical Documentation & Diagnoses
Trinda Health’s patented healthcare quality algorithm identifies hospital encounters that could benefit from more comprehensive coding to improve quality measures, then presents them to CDI specialists in a prioritized worklist.
Our technology adjusts to the ongoing changes in ranking methodologies to forecast hospital ranking enhancements with a focus on the accuracy of medical diagnoses based on complications or comorbidities associated with chronic and acute conditions.
2. Increase Patient Classification & Risk Adjustment Accuracy
An overwhelming 86% of DRGs can be elevated from base to CC, base to MCC, or CC to MCC.
Our healthcare CDI software identifies the HCC categories with the highest risk adjustment opportunity, forecasts the incremental lift in quality based on potential promotable DRGs, and clearly displays opportunities by DRG, provider, service line, and quality measure.
3. Optimize Quality Reporting & Reimbursement
Our evidence-based algorithm understands the risk models for payment and reverse engineers the various quality rating calculations to provide you with a clear roadmap to quality and financial gains.
The Trinda Health CDI software eliminates the human error in data analysis and allows CDI teams to scale the discovery of improvement opportunities. With enhanced clinical documentation, hospitals can prove the quality of care delivered and drive value-based payments.
Why Trinda Health is Different
We Make Healthcare Quality More Transparent
Our healthcare quality improvement software gives CDI teams and hospital leaders unprecedented insight into quality calculations and rating systems so your organization can gain a competitive edge.
We helped transform a large midwestern academic medical center’s rating from 3 stars to 5 in just 18 months by showing them the specific encounter and coding categories that had the greatest potential to impact quality ratings, so they knew exactly where to focus their efforts.
We Transform Complex Data into Actionable Priorities
Our tool generates a comprehensive dataset daily and pinpoints clinical variables with the potential to improve health system quality and reimbursement. The result is improved documentation, enhanced coding, adjusted risk, stronger diagnosis groupings, and more accurate reimbursement.
We Help Capture More Revenue
Our CDI software directly impacts financial performance through value-based purchasing and the hospital readmissions reduction program, and indirectly through contract negotiation and technology enablement. Our patented algorithm and automated daily updates give CDI teams the insights and information they need to improve coding accuracy, revenue integrity, and quality measures.



